Breast Reconstruction
There are several factors to consider in the breast reconstruction process after cancer or other breast disease.
Although breast reconstruction techniques have advanced considerably in the last years, it must be kept in mind that the reconstructive process is not simple. Very good results are achieved, yet without being perfect.
These procedures not only enable the patient to restore her lost body harmony, but also, and this is as important: allows her to restore her emotional well-being. The reconstruction can begin immediately after the mastectomy (immediate), or time after it (differed).
The reconstruction is conditioned to several factors, such as breasts size and shape, extirpated tissues, general health state, lifestyle, emotional state and patient expectations, among others things.
As plastic surgeons, we inform the patient about the different reconstruction possibilities and we select the best option together with her and the mastologist. Each case is unique.
Basically two methods of breast reconstruction exist. The one that uses aloplastic materials (breast implants), and the reconstruction via autologous tissue (flaps) from the same patient.
The first option consists of the positioning of silicone or saline implants underneath the skin, subcutaneous cellular tissues and thoracic muscles, recreating the shape and appearance of the breast.
The second transfers skin, fatty tissue and muscle from the abdomen or the back (less frequently from other areas of the body), to the region of the extirpated breast. In some cases both possibilities are combined.
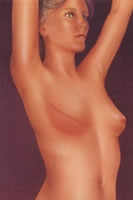
In patients with elastic, healthy skin and a small contralateral breast, it can be sufficient with the implant placement to equal the contralateral breast.
But if those are not the conditions, the expansion or stretching of tissue for some time is required, by means of the progressive action of an “expander” that is gradually filled with saline through a remote or internal valve in the device.
The process of tissue expansion is similar to the one which takes place in the feminine abdomen during the pregnancy. After 3 to 6 months, by means of a second intervention, the expander is replaced with the definitive implant.
There´s also the possibility of placing definitive “expander-implants”, that combines both functions with only one surgery.
Traditionally the tissue expanders and the definitive implant have been round and with a smooth surface. Lately, others with anatomical form have been developed, simulating the breast shape, and a textured surface, diminishing the incidence of retractable capsule (“hardening”), one of the complications of the procedure. There are also in the market silicone gel implants but with polyurethane shell.
The reconstructive method by means of an expander and implant, is spread widely. In general it doesn´t require additional scars to those of the mastectomy and is extremely versatile.
If it takes place immediately after the mastectomy, it does not prolong the surgery for more than 20 minutes. If the implant or expander placement is deferred, it can be performed as an ambulatory procedure.
Patients must know that they must go to the doctor’s office several times for the expansion sessions of the device. This can cause discomfort or pain temporarily, as well as asymmetry during this period.
Women who received radiotherapy associated to the mastectomy present greater percentage of failure with this procedure.
The expansion and implant can present other complications, like retractable fibrous capsule (hardening), infection, extrusion, valve malfunction and deflation, malposition, asymmetries, etc-.

The shaded zone indicates
the area where the tissue
expander is placed.
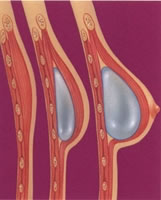
The expander is filled
progressively with saline
to make the skin stretch.
Reconstruction of the breast
volume and shape after
the replacement of the expander by
a definitive implant.
The reconstruction by means of the patient’s own tissues (autologous), is based on the transference of a skin segment, fatty tissue and muscle from a part of the body to the breast region.
The most spread surgery nowadays, is the one that transfers an inferior abdominal dermo-fat flap to the thorax, TRAM (transverse rectus abdominis muscle).
The TRAM can be pediculated, taking the straight muscle; or it frees, if the transference is made with microsurgical technique.
This method presents obvious benefits, as no devices are inserted into the body, making it possible for the reconstruction of a breast with a shape, fall and very natural feel at touch.
Likewise it reduces the amount of excess abdominal tissue significantly, leaving the abdomen flatter.
It is an ideal option in patients with important scars in the chest area, very thin dermo-fat flaps, and/or who have dealt with radiotherapy. Also for cases of reconstruction of great breasts, patients who don´t wish synthetic materials in their bodies, who don´t want a reduction practice made to them and/or a pexy in the contralateral breast and for failed attempts of reconstruction with other methods.
It is necessary to clarify that it is a surgery of certain magnitude. It requires general anesthesia and in-patient stay. The operation is performed in one time. It leaves an abdominal scar similar to the one left in an abdominal aesthetic surgery.
One of the complications that can take place after a TRAM is the weakness of abdominal wall, (laxity or eventration). This is less frequent with a flap transferred in a “free” form with microsurgery; and even less with a technique that doesn´t use muscle in flap, denominated “piercing”, because of the individualization of the tissues, by means of which the pad flap is prepared with skin and fatty tissue, avoiding to take muscle in it.
The microsurgical alternative requires specific infrastructure and a medical equipment highly trained in this technique, because a failure implies the total loss of the flap.
The very obese patients, with history of important diseases or smokers aren’t good candidates for this procedure. A series of risk factors exists that they make a distinction in patients to diminish the possibilities of post-operating complications.

Tissues taken from the
abdomen and tunneled for the
breast reconstruction

Abdominal tissue transported to the
breast region y sutured.
Closing of the abdomen.
Resulting scars
after the surgery
with abdominal tissue.
TRAM
Another reconstructive procedure with autologuos tissue, is the one that uses wide dorsal muscle with or without a pad of adjacent skin.
This technique almost always requires the use of an implant to obtain breast volume, considering that the flap has little thickness. The doctor can design the pad of skin necessary to cover the defect in the neobreast. It is possible to transport more or less wide dorsal muscle, adapting this to the needs of the defect to cover, achieving a complete muscular cover for the implant by suturing the dorsal muscle to the pectoral one.
This procedure can leave some depression at the donor´s site and a more or less visible scar. We try to make it where it could hidden with a bra.

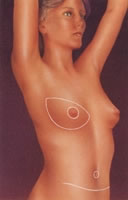
The shaded area indicates
the area to reconstruct.

Transposed tissues to the
anterior area of the thorax,
with the inclusion of an implant
to reshape the new breast

Resulting scars
after the reconstruction with
dorsal muscle and implant.
All the techniques must be completed with the reconstruction of the areola-nipple set. This usually requires a small intervention with local anesthesia.
Sometimes it is necessary to treat the contralateral breast, performing in some cases a breast augmentation, a reduction or a pexy, with the intention of achieving breast symmetry, one of the most important goals to consider in breast reconstruction.
 +54 (011) 4861-9794 +54 (011) 4864-6018
+54 (011) 4861-9794 +54 (011) 4864-6018 English
English Español
Español 




